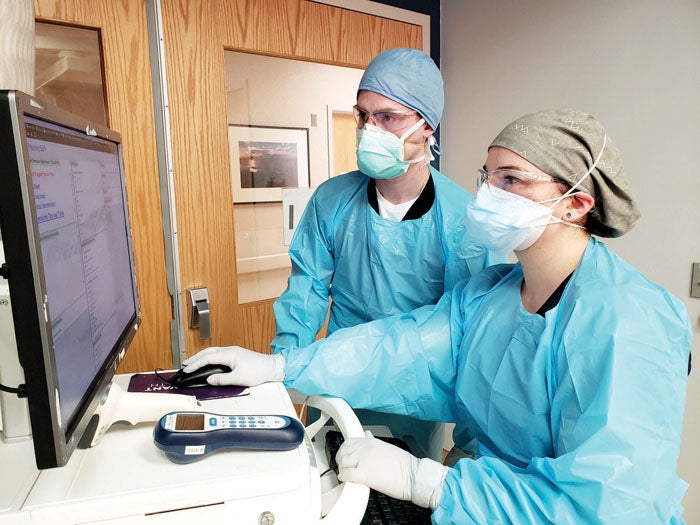
Registered nurses Zach Matthews, 25, and Jessica Walls, 29, serve together on the ICU’s rapid response team at Novant Health Forsyth Medical Center in Winston-Salem. They both work in the COVID-19 unit, and shared what the last month has been like.
‘It’s my purpose’
Matthews says there is a lot more stress and anxiety in the hospital right now.
“I can sense it in our patients,” he said. “But personally I am energized to come to work. And I’ve noticed that everyone on our team has been coming in more determined than ever to help our patients get through this pandemic.”
As an ICU nurse, even before the pandemic, Matthews is used to spending his days caring for the critically ill. And he credits his mother, a wound ostomy nurse at the hospital, for inspiring him to go into medicine.
“Taking care of wounds is hard work,” he said, “But getting to watch her over the years and see the fulfillment that she gets out of helping people is what pushed me into the field.”
Matthews went on to earn his nursing degree from the University of North Carolina at Greensboro, and joined the ICU team at Forsyth Medical Center in 2017.
At work, he can be hard to recognize. Like soldiers going into battle, he and his fellow ICU nurses each don their personal protective equipment (PPE) before entering the COVID-19 unit. This process takes several moments to carefully strap on a head covering, eye shield, two protective masks, a gown and gloves, then they check and recheck themselves before entering a patient room.
“In the past we used to be able to just run in and out of rooms,” he said. “But this pandemic has forced us to be more creative in our approach.”
One of those changes includes relocating each IV pole outside of the patient’s room. If something beeps, and a change needs to be made, nurses can now make those changes safely without having to suit up to enter the room. Another change has come in the form of a switch to cluster care nursing. This approach is more commonly performed on the maternity floor of the hospital to allow new moms to have more time to sleep. The idea is to group daily nursing care tasks together to improve efficiency and better protect team members and patients.
“I feel like God has put me in this place right now for a reason,” he said. “And it’s my purpose in life to help these patients.”
‘Always do one thing better’
The COVID-19 pandemic has also inspired Walls to stay focused on her goals.
“Every day I always want to do one thing better than the day before,” she said. “And when you are treating patients that have the coronavirus, there is no room for complacency.”
Walls’ interest in medicine started in high school after she took a junior explorers class that allowed her to shadow nurses at Forsyth Medical Center. She went on to complete her nursing degree at the University of North Carolina at Wilmington, and joined the ICU team in 2017.
“I enjoy working in the ICU because we get to see patients at their worst moments in life and try our best to help them recover,” she said. “The only difference today is that we are all more aware of what is going on in the world right now, and I think it is important for us to remember to stop and breathe.”
Today she is thankful for her parents, the support of her work family and her fiancé, a fellow ICU nurse. “I’ve learned through this process that we don’t need everything we think we need,” she said. “The things we used to take for granted, I don’t take for granted anymore.”
‘We talk with a smile now’
Ordinarily, Ruth Exis is an assistant daytime nurse manager on the neurology floor at Novant Health Presbyterian Medical Center in Charlotte. She’s still on the same floor, but it’s been converted to a wing dedicated solely to caring for “intermediate” COVID patients. Exis’ team cares for patients who are sick but don’t need a ventilator. Patients requiring a ventilator are in the ICU.
Some patients are scared. They see the news on TV; they know about the rising death toll. They can’t have visitors. Exis and her team do what they can to bridge the gap. Patients weren’t allowed to bring their devices from home. So, some nurses began using their own personal devices to let patients communicate with their families. Exis asked her leader, Jason Cooke, director of nursing critical care and neurosciences at Novant Health Presbyterian Medical Center, about getting an iPad for their floor that nurses could take from room to room.
“He made it happen that day,” she said. “It was the biggest blessing. Everything we’ve asked for, our senior leaders have delivered.”
That includes PPE. That’s a necessity, but it interferes with the relationship between provider and patient. “They can’t see our faces,” Exis said. “They don’t even know what we look like.” Nurses and doctors are so shielded, they don’t always even recognize each other.
“We’ve had to get creative about how we deliver care,” Exis said. “We talk with a smile now.” Patients can’t see it, but they hear it.
“It’s a totally different kind of care we’re giving,” Exis continued.
Yet, Exis said there’s an energy on her floor she’s never felt before. “Teamwork has never been more important,” she said. “These nurses know the whole team has got their back. There’s a new level of trust that has brought a positivity to our unit — one you can feel.” She calls her team “heroic” and said she’s been “amazed by their stamina and compassion.”
What’s more, patients are getting better and being discharged. Each patient who goes home is another team triumph and dose of good cheer.